As California experienced a surge in COVID cases in January, our Western Division Ambulatory Care Coordination pivoted to COVID surge support, concentrating on patients being discharged from hospitals while also supporting COVID-positive patients in the clinic. A new workflow was needed to address the growing number of patients being discharged, as the team shifted its focus from daily operations to problem-solving to meet the needs of the moment.
Getting Patients the Care They Need
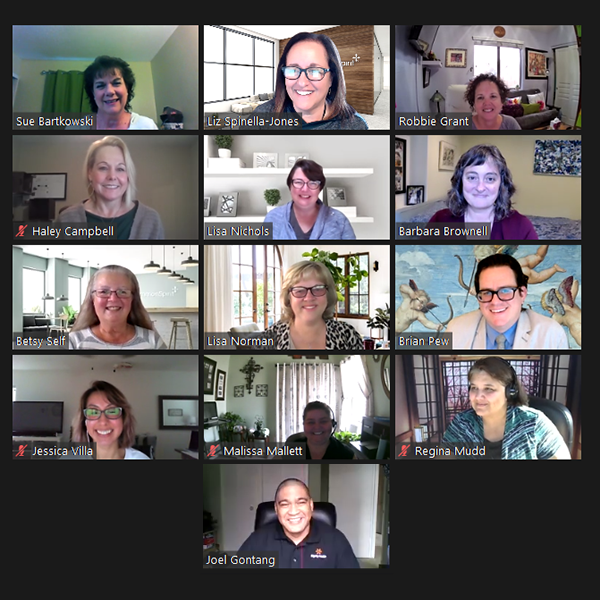
Every discharged COVID patient receives a call from a Registered Nurse Care Manager. To ensure patients were getting the care they needed, Western Division team members utilized a payer-agnostic approach and focused on identifying those patient needs and then looked to the local markets for assistance, says Liz Spinella-Jones, System Director, Clinical Care Coordination.
The team was given the freedom to develop workflows together as the situation developed — and to remain fluid and flexible until they settled on a system that worked. Weekly huddles became daily, so team members could share their concerns, raise any issues and solve them together.
“It’s really helped all the teams get to know each other across the Western Division, which has been a beautiful thing,” Spinella-Jones says.
Measuring Success
The resulting patient success stories demonstrate the needs the team has been able to help address. Here are a few brief examples:
- Food insecurity: A 23-year-old male with disabilities was recuperating well but mentioned to his case manager that he had little to no food (he had not disclosed this during hospitalization). The case manager connected him to a disability agency and a food hotline, following up with the patient to confirm food was being delivered to him via the hotline.
- Missing medications: A 30-year-old female received nebulizer meds but couldn’t figure out how to take them. The care team member discovered she had not received the actual nebulizer and reached out to the hospitalist, who put in orders for treatment. By the next day, she had received the nebulizer and was able to use it properly.
- DME disconnect: A 73-year-old male had been waiting for months for a CPAP machine but had not received it. The case manager called his physician’s office and determined that the DME supplier had the wrong number for the patient. The case manager helped the patient get the DME he required, and the patient was grateful for the follow-up care.
- COVID education: A surprising number of patients are receiving misinformation from family members, news sources and even medical sources regarding COVID-19. For example, many are surprised to learn that they are not immune after being diagnosed with COVID, so this effort has provided an opportunity for the teams to offer patient education — from a trusted source on which they already rely.
The team has received excellent feedback on the COVID-positive follow-up calls, with patients expressing their gratitude and relief that someone is watching out for them.
While multiple teams contributed to the overall success of this effort, special recognition goes out to the following team members for their dedication:
- Susan Bartkowski and Robbie Grant for taking on the daily discharge lists and devising a system to make those lists actionable.
- The Frontline Triage RN team — Dominique Fairbank, Kathy Holton and Aida Munoz De Ortiz — for taking on the triage for payer-agnostic hospital discharges for COVID-positive patients and helping to develop the process.
- Local Market RNs — Charisse Sayson (Kern), Pinder Maheru (Stockton/Merced/Sequoia/San Francisco), Sarah Wilson (Redding), Cheryl Demonner PA (Santa Cruz), Bev Cruz and Aida Munoz (IE) — for working across the markets with the Triage team and each other to help the members and our team.
Spinella-Jones and the team also are aiming to ensure that this work will live on.
“We’re hoping to take some of the things we’ve learned from this and embed them into our everyday care coordination,” she says. “Now that we’ve developed this workflow and these processes, we can use them to address other needs as well.”