In the beginning, it was blood-pressure spikes that worried Ken Huebel, whose doctor wrote a prescription for medicine to help manage his condition. Over time, the retired accountant noticed he would get out of breath, so his doctor ordered an exercise stress test.
An exercise stress test checks how someone’s heart handles physical exertion. The veteran’s test results indicated a possible blockage in the arteries feeding his heart. He underwent a cardiac catheterization to check the internal workings of his heart, where they found Huebel’s left anterior descending (LAD) artery was 100% blocked. That’s the artery that carries nearly half the blood to the heart.
The 78-year-old resident of Shenandoah, Texas, was told they couldn’t open the artery with a stent, and he needed surgery. His cardiologist recommended Dr. Vivek Patel, who performs robotic-assisted coronary artery bypass surgery and traditional bypass surgery, at St. Luke's Health-The Woodlands.
“He said he would send his own mother there, so he's apparently really good at the robotic surgery,” Huebel said.
Huebel’s LAD had been completely blocked for several months, but his other blood vessels had made channels, known as collaterals, to keep blood flowing, said Dr. Patel, assistant professor of surgery in the Division of Cardiothoracic Surgery at Baylor College of Medicine. This is called collateral circulation. It happens when a network of tiny blood vessels form or become active when the normal blood flow through a major artery is blocked or narrowed. Without stents or surgery, Huebel’s condition would deteriorate, Dr. Patel said.
“The only other option is to do nothing, in which case his symptoms would be worse over time. The (heart) muscle dies if we don’t get good blood supply to it and, eventually, his heart pumping function would decline over time,” Dr. Patel said.
Huebel underwent the successful surgery in early March, where Dr. Patel made three small keyhole incisions on the left chest, used an internal mammary artery for the bypass and did not even have to use the heart-lung machine (cardiopulmonary bypass), which is used for most traditional open-heart surgeries. The device temporarily replaces the functions of both organs, allowing surgeons to operate on a still heart and helps ensure the patient receives oxygenated blood. Avoiding the heart-lung machine translates to less risk of blood transfusions and stroke, faster recovery times and less pain, Patel said.
The robot is an instrument Dr. Patel controls during surgery that allows him to get into smaller spaces without making a big incision.
Huebel went home with a medication regimen that included aspirin to help prevent blood clots, statins for high cholesterol and beta blockers to help with high blood pressure. He also began cardiac rehab, which he liked because nurses watched and monitored him while he was exercising. Still, he would sometimes overdo it, leading to pain.
Dr. Patel said that as patients become more confident in their exercise routines after several weeks, they might push themselves too hard. This can result in some incisional or musculoskeletal pain.
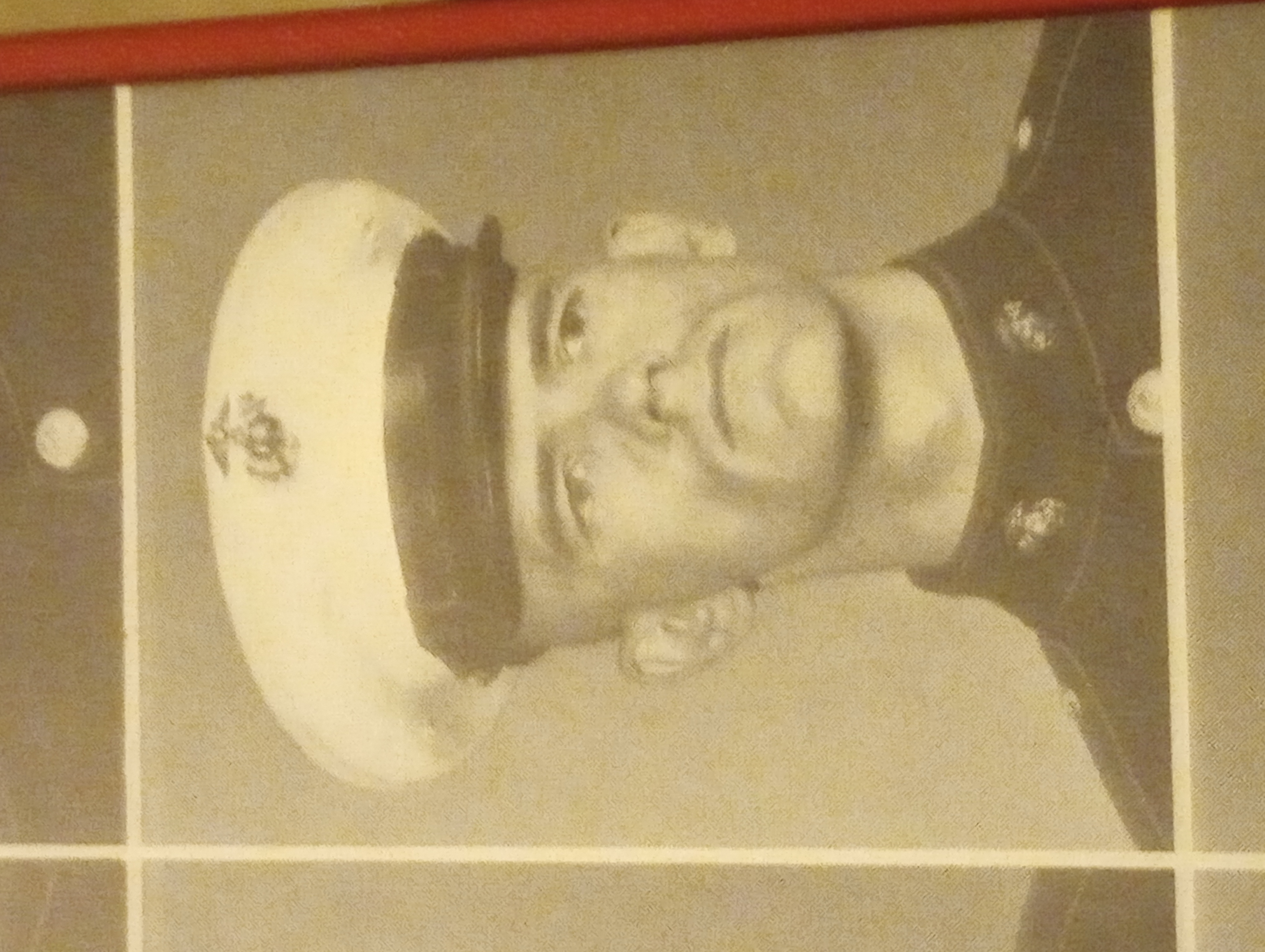
For now, Huebel is happy to be able to bowl again, a sport he picked up in his youth. He and his wife are both regular players and take part in a bowling league. Huebel also played when he was in the U.S. Marine Corps during the Vietnam era when he was stationed in Yuma, Arizona. There he won the All-Marine Tournament.
He has even bowled a few perfect games, scoring 300 points with 12 consecutive strikes.
Huebel said his recovery is coming along well now.
“Feeling much younger than my age again,” he said. “The health issues I had for the past year were starting to make me feel older. Now that I’m getting healthier with the exercise program, I’m back to feeling more like I did before.”