What is an Achilles tendon tear?
An Achilles tendon tear—sometimes called a rupture—can be partial or complete. Partial tears may cause no symptoms. But complete tears cause pain and sudden loss of strength and movement. Middle-aged adults doing sports activities are more likely to get this kind of injury. Tears also happen in older adults.
What are the symptoms of an Achilles tendon tear?
Symptoms of an Achilles tendon tear may include:
- A sudden, sharp pain that feels like a direct hit to the Achilles tendon. There may be a pop when the tear occurs. This may be followed by swelling and bruising.
- Heel pain. (It may be severe.)
- Not being able to go on tiptoe with the hurt leg.
If you have only a partial tear of the Achilles tendon, you may have near-normal strength after the injury. Some people with partial tears may not have any symptoms.
Achilles Tendon Injury
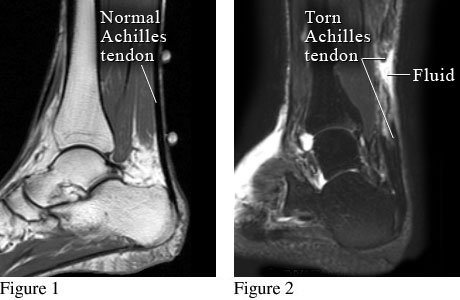
Courtesy of Intermountain Medical Imaging, Boise, Idaho.
Figure 1 shows magnetic resonance imaging (MRI) of a normal heel and Achilles tendon. Figure 2 shows a torn Achilles tendon with fluid collected at the site of the tear.
How is an Achilles tendon tear treated?
Treatment for an Achilles tendon tear includes:
- Surgery. This is often used to reattach the ends of a torn Achilles tendon. Surgery works best when you have it soon after your injury. Surgery is followed by rehabilitation (rehab). Recovery may take months.
- Immobilizing your leg. This prevents movement of the lower leg and ankle. It allows the ends of the Achilles tendon to reattach and heal. It may take as long as 6 months to completely heal the tendon. A cast, splint, brace, walking boot, or other device may be used. This treatment is followed by rehab.
Treatment takes time, but it usually works. Most people can return to sports and other activities.
If you are healing from an Achilles tendon tear, don't smoke or use other tobacco products. Smoking slows healing. This is because it decreases blood supply and delays tissue repair.
How can you care for yourself when you have an Achilles tendon tear?
You can do several things to help you heal and strengthen your Achilles tendon. Avoid activities that strain the tendon. Ice the tendon and take over-the-counter pain relievers to reduce pain. Do gentle exercises like calf stretches. Wear supportive shoes that cushion your heels. If your doctor suggests it, wear a night brace.
©2011-2026 Healthwise, Incorporated
