Electrical cardioversion for a fast heart rate: Overview
Electrical cardioversion is a procedure in which a brief electric shock is given to the heart to reset the heart rhythm back to its normal, regular pattern (normal sinus rhythm). The shock is given through patches applied to the outside of the chest wall. In some situations an external defibrillator, which has paddles, might be used.
Usually, the person is sedated. If the person is conscious, medicine is given to control pain and to cause the person to relax to the point of being nearly unconscious during the procedure.
Why is electrical cardioversion done?
Cardioversion is used:
- As a non-emergency procedure to stop a heart rhythm problem that has not stopped on its own. These heart problems include atrial fibrillation, atrial flutter, and supraventricular tachycardia.
- As an emergency procedure to stop a fast heart rate that is causing low blood pressure or severe symptoms. These heart rate problems include atrial fibrillation, atrial flutter, supraventricular tachycardia, and ventricular tachycardia.
Electrical Cardioversion
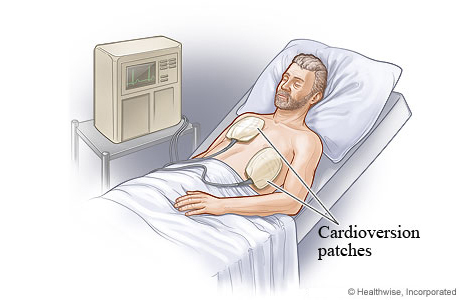
Before electrical cardioversion, you will get medicine to make you sleepy. You should not feel any pain. Then your doctor places patches either on your chest or on your chest and back. The patches send an electric current to your heart. This resets your heart rhythm.
After electrical cardioversion: When to call
Call 911 anytime you think you may need emergency care. For example, call if:
- You passed out (lost consciousness).
- You have symptoms of a heart attack. These may include:
- Chest pain or pressure, or a strange feeling in the chest.
- Sweating.
- Shortness of breath.
- Nausea or vomiting.
- Pain, pressure, or a strange feeling in the back, neck, jaw, or upper belly or in one or both shoulders or arms.
- Lightheadedness or sudden weakness.
- A fast or irregular heartbeat.
- After calling 911, the operator may tell you to chew 1 adult-strength or 2 to 4 low-dose aspirin. Wait for an ambulance. Do not try to drive yourself.
- You have symptoms of a stroke. These may include:
- Sudden numbness, tingling, weakness, or loss of movement in your face, arm, or leg, especially on only one side of your body.
- Sudden vision changes.
- Sudden trouble speaking.
- Sudden confusion or trouble understanding simple statements.
- Sudden problems with walking or balance.
- A sudden, severe headache that is different from past headaches.
Call your doctor now or seek immediate medical care if:
- You feel dizzy or lightheaded, or you feel like you may faint.
- You have a fast or irregular heartbeat.
Watch closely for any changes in your health, and be sure to contact your doctor if you have any problems.
©2011-2026 Healthwise, Incorporated
